Damage to the retina caused due to long-standing diabetes is called Diabetic retinopathy.
Poor control of diabetes and long-standing diabetes are the main causes of diabetic retinopathy.
Diabetic retinopathy typically has no symptoms until it is too late. There are leaky blood vessels in the retina in diabetic retinopathy. If the blood vessels become very fragile, this can result in sudden bleeding into the vitreous. This sudden bleeding can be triggered by simple activities like sneezing, coughing or straining. This bleeding is typically painless and will result in sudden obscuration of vision in a patient who has had diabetes for a long duration. Gradually over a period of many weeks and months the blood will clear from the vitreous and vision may be restored. Usually this can progress into something called tractional retinal detachment, if it is not treated effectively.
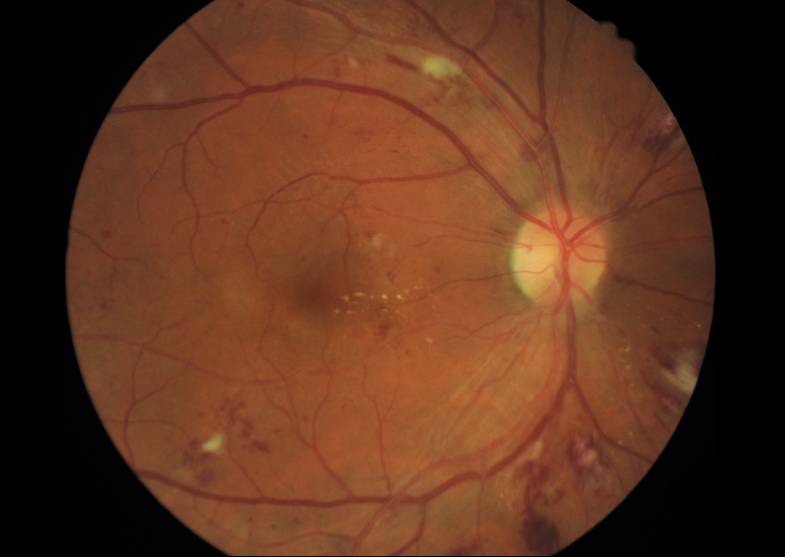
At Magna, we use a fundus photograph to recognise the presence of Diabetic Retinopathy. This is a test where we acquire photographs of the retina using a sophisticated camera. The photographs are then read by eye specialists remotely and reports are given to the patient. In the fundus photograph the retina specialist looks for Micro aneurysms or small out pouching in blood vessels which are seen normally in the retina. These small out poaching or weakening in the walls of blood vessels can sometimes rupture causing small bleeding within the retina called hemorrhages. A trained retinal surgeon can then measure the amount of abnormalities in the retina and then treat the retinopathy as mild NPDR, moderate and PDR or severe and Pedia. Once the disease progresses beyond this point, new blood vessels start forming in the retina. This is called new vascularisation. At this stage, we call the condition as proliferative diabetic retinopathy or PDR.
Diabetic retinopathy usually manifests itself first up to 5 to 10 years following the diagnosis. In patients with type one diabetes, screening should be started five years after the diagnosis of disease. In type2 diabetes the onset of disease is not very clear and we should screen for diabetic retinopathy at diagnosis in all patients with type2 diabetes.
Diabetic retinopathy has specific treatments aimed at preventing new vascularisation or destroying vessels which can cause bleeding.
At Magna, once we recognise that a patient has diabetic retinopathy, we take full precaution to make sure that the patient’s glucose control is improved. Glycaemic control is one of the most important ways through which diabetic retinopathy can be prevented or improved . Certain medications like fenofibrate statins are effective in reducing the progression of diabetic retinopathy. Good blood pressure control also helps in preventing the progression of diabetic retinopathy as well as management of iron deficiency anemia.
We are a healthcare group founded by endocrinologists. Our vision is to provide personalized and evidence based health care for patients with Endocrine Disorders?.
Common disorders include Diabetes, Obesity, Thyroid dysfunction and PCOS. All these disorders require repeated examination by the doctor, quality laboratory evidence based prescribing, nurse /dietitian educators, podiatrist, preventive cardiologist, urologist and many more professionals. We endeavor to bring this integrated healthcare team under one roof at an affordable cost to our patients with endocrine problems.
All the information of the website is published in good faith and for general information purpose only. Any action you take upon the information you find on the website is strictly at your own risk. We will not be liable for any losses/ or damages in connection with the use of our website. By using our website, you hereby consent to our disclaimer and agree to its terms.
